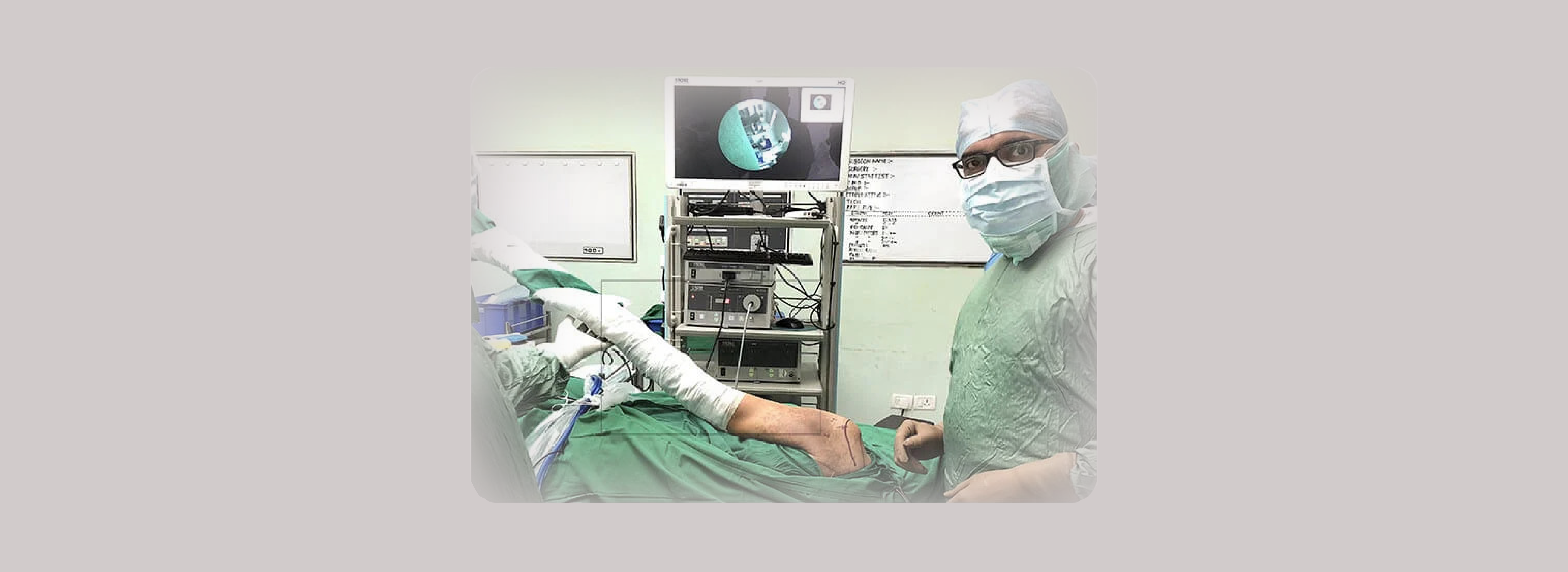
SHOULDER ARTHROSCOPY SURGERY
Shoulder Arthroscopy Surgery has revolutionised the treatment of shoulder pathologies. It had been performed since 1970s, however in the last two decades, with the advent of newer instrumentations and technology, the shoulder surgeons across globe have been able to treat more and more number shoulder ailments with this minimally invasive technique. It is not just cosmetically superior and safe, but also allows access to those areas of shoulder joint which would often be inaccessible by routine open surgical methods. After Shoulder Arthroscopy Surgery the recovery of the patient has been much easier and faster than once thought possible by traditional open surgery.
It is usually performed under general anaesthesia along with brachial plexus block which nearly eliminates pain in the immediate post-operative period.
What are the indications of Shoulder Arthroscopy Surgery?
With technological advances, Shoulder Arthroscopy Surgery has evolved and progressed to such an extent that we are able to treat number of clinical conditions more effectively than ever before. It provides better surgical precision, better cosmesis, rapid recovery and thereby more patient satisfaction
Following are the indications for Shoulder Arthroscopy Surgery:
- Shoulder Instability
- Rotator cuff tear
- Slap tear
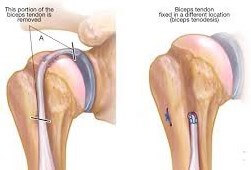
- Biceps tendon injuries
- Biceps tendon tears
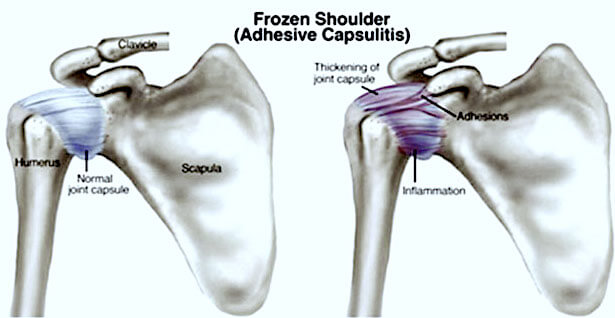
- Frozen Shoulder
- Subacromial Impingement Syndrome
- Loose bodies in the shoulder joint
- Greater tuberosity fractures of proximal humerus
- Acromioclavicular joint separation
- Suprascapular nerve release
- Shoulder(Paralabral) Cysts
What is shoulder instability?
This is the condition in which the shoulder joint dislocates, usually as a result of an injury. Due to poor healing of the soft tissue, often there is a recurrence. The diagnosis is done by history and clinical examination and the lesion is best identified by MRI scan. If the shoulder joint has dislocated multiple times, then there is bone loss of the glenoid cavity (Tee or cup of the joint) that needs to be quantified by CT scan to decide upon the best procedure to be offered to the patient.

In the cases without significant bone loss, Arthroscopic Bankart’s Repair surgery with or without Remplissage procedure is performed. When there is significant glenoid bone loss a bone augmentation procedure such as Laterjet surgery is performed.
What is Arthroscopic Bankart’s Repair Surgery?
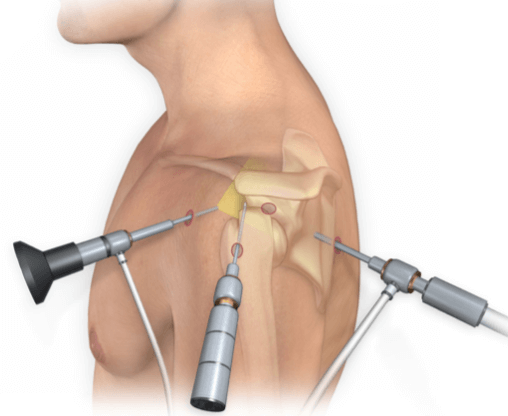
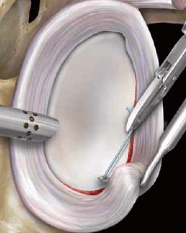
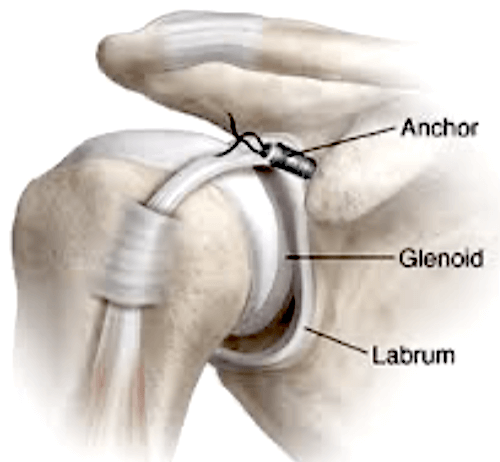
The shoulder joint (glenohumeral joint) is a ball and socket joint, where the head of the humerus bone attaches to the shoulder socket (glenoid cavity). The shoulder socket is extremely shallow and therefore needs additional support to keep the shoulder bones from dislocating. The labrum, a cuff of cartilage that encircles the shoulder socket, helps serve this purpose by forming a cup for the humeral head to move within. It provides stability to the joint, enabling a wide range of movements.
The labrum can sometimes tear during a shoulder injury. A specific type of labral tear that occurs when the shoulder dislocates is called a Bankart tear. This is a tear to a part of the labrum called the inferior glenohumeral ligament and is common in younger patients who sustain a dislocation of the shoulder. A Bankart tear makes the shoulder prone to repeat dislocation in patients under 30 years of age.

An Arthroscopic Bankart repair surgery is indicated when conservative treatment measures do not improve the condition and repeated shoulder joint dislocations occur.
During an arthroscopic Bankart procedure, The surgeon makes a few portals over your shoulder joint. The surgeon then uses small surgical instruments through the other tiny incisions to trim the edges of the glenoid cavity. Suture anchors are then inserted to reattach the detached labrum to the glenoid. The tiny incisions are then closed and covered with a bandage.

Arthroscopy causes minimal disruption to the other shoulder structures and does not require the surgeon to detach and reattach the overlying shoulder muscle (subscapularis) as with the open technique.
- After the surgery, the patient spends about an hour in the recovery room.
- Shoulder exercises are started as the pain is tolerated in the following days.
- The patient is allowed to perform his daily activities as tolerated, but without lifting objects heavier than a plate or glass.
- The arm may be placed in a sling for three weeks to restrict use of the operated shoulder.
- The patient may resume light low-risk activities, like jogging and swimming 8 to 10 weeks after surgery, and may be advised to avoid contact sports for some time.
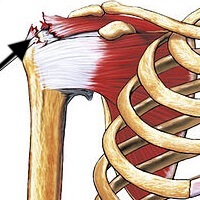
What is rotator cuff tear and how is it treated arthroscopically?
The rotator cuff is a group of four muscles on top of the shoulder joint. The individual muscle names are subscapularis, supraspinatus, infraspinatus and teres minor. They are the key muscles responsible for the smooth functioning of the shoulder. The rotator cuff can get inflamed (tendinitis) or torn as a result of injury or degeneration.


Most tears occur in the supraspinatus tendon, but other parts of the rotator cuff may also be involved. In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
There are different types of tears.
- Partial tear:This type of tear is also called an incomplete tear. It damages the tendon, but does not completely sever it.
- Full-thickness tear:This type of tear is also called a complete tear. It separates all of the tendon from the bone. With a full-thickness tear, there is basically a hole in the tendon
The most common symptoms of a rotator cuff tear include:
- Pain at rest and at night, particularly if lying on the affected shoulder
- Pain when lifting and lowering your arm or with specific movements
- Weakness when lifting or rotating your arm
- Crepitus or crackling sensation when moving your shoulder in certain positions
Treatment
Depending upon the tear pattern the patient is offered conservative or surgical treatment options by the surgeon. If the symptoms are significant, an arthroscopic repair of the torn tendons is performed. Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus bone. A partial tear, however, may need only a trimming or smoothing procedure called a debridement. A complete tear is repaired by stitching the tendon back to its original site on the humerus.


There are various techniques described for rotator cuff repair such as single row or double row repair. The arthroscopic repair uses “anchors” which are tiny screw like implants with inbuilt sutures to help reattach the rotator cuff on to the tuberosity of the humerus. Your surgeon Dr. Fayaz Memon will discuss with you the best procedure to meet your individual health needs.
Outcome
The majority of patients report improved shoulder strength and less pain after arthroscopic rotator cuff repair surgery.
Factors that can alter the likelihood of a satisfactory result include
- Poor tendon/tissue quality
- Large or massive tears
- Poor patient compliance with rehabilitation and restrictions after surgery
- Very old patient age
- Smoking and use of other nicotine products
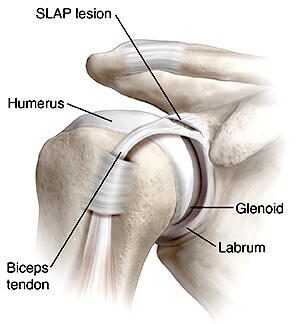
What is a SLAP tear and how is it treated?
What is a SLAP tear?A SLAP tear, or Superior Labrum Anterior and Posterior tear, is a type of shoulder injury. When a SLAP tear occurs, the superior portion of the labrum of the shoulder is damaged. The superior portion of the labrum is attached to the biceps tendon. The labrum is a cup-shaped rim of firm, fibrous tissue that cushions the socket of the shoulder joint, stabilizes and reinforces the ball and socket of shoulder joint
What are the causes of a SLAP tear?
- Repetitive use of the shoulder in throwing sports
- Rapid over the shoulder or overhead movement
- Shoulder dislocation
- Acute trauma from a motor vehicle accident
- Falling onto an outstretched arm in front of or to the side of the body
- Falling on the shoulder
- Forceful pulling of the arm
- Lifting heavy objects
- Degeneration, or the wearing down of the labrum
What symptoms are associated with SLAP tears?
- Deep, aching pain
- Popping, clicking, catching, locking or grinding in the shoulder
- Decreased range of motion
- Shoulder instability
- Pain when lifting or carrying objects
- Pain when moving the arm or shoulder
- Decreased shoulder strength
Treatment
Initial treatment methods for SLAP tears are typically nonsurgical. Depending on the injury, the doctor may recommend anti-inflammatory medication to reduce pain and swelling, followed by physical therapy exercises designed to strengthen the shoulder and restore range of motion and function.
When a nonsurgical treatment does not improve symptoms or the patient has sustained a more severe injury, arthroscopic surgery may be recommended. Arthroscopic shoulder surgery is a procedure that allows surgeons to insert a miniature camera into a patient’s shoulder through small incisions. Once the camera is inserted, the surgeon is able to see its feed displayed on a video monitor screen. By referring to the camera’s feed, the surgeon is able to determine which surgical measures to take. Surgical repair may involve removing the torn portion of the labrum or reattaching the torn portion of the labrum with stitches. Your surgeon Dr. Fayaz Memon will determine the best method of repair based on the tear pattern and your individualised needs.
What are Biceps tendon injuries?
The biceps muscle has two tendons that attach it to the bones of the shoulder and one tendon that attaches to the radius bone at the elbow. Injuries to the muscle include tendonitis and tendon tears. The biceps muscle is located at the front of upper arm. The muscle has two tendons that attach it to the bones of the scapula bone of the shoulder and one tendon that attaches to the radius bone at the elbow. The tendons are tough strips of tissue that connect muscles to bones and allow us to move our limbs.
Injuries to the biceps tendons include:
- Proximal biceps tendinitis at shoulder
- Proximal biceps tendon tear at shoulder
- Distal biceps tendonitis and tear at the elbow
What is biceps tendinitis?
At times overuse of tendons make them sore and painful. This is caused by micro tears in the tendon and it is called tendinitis. Tendinitis can occur because of repetitive motion. For instance, in swimmers, tennis players and golfers are at risk for tendonitis in their shoulders, arms and elbows. Tendinitis can also occur because of a sudden, serious load to the tendon. One can get biceps tendonitis in the shoulder or at the elbow. It is unusual to have tendonitis in both places at the same time. In the shoulder, biceps tendonitis can occur at the same time as rotator cuff.
How is biceps tendinitis treated?
Although biceps tendonitis can be painful, if properly treated early it can usually be resolved completely.
- Cold packs or ice will reduce swelling and pain caused by tendonitis.
- Painkillers such as aspirin or ibuprofen will help relieve swelling and pain.
- Rest to part
- In some cases physiotherapy may be recommended.
- In severe cases of tendinitis without a tear, local steroid injection may offer relief of pain and halt the inflammatory process and get the tendon back on a path of healing.
Most patients who have had surgery for tendonitis can move their arms without pain and regain a full range of motion.
What are biceps tendon tears?
In cases of constant overuse, a tendon may fray and eventually tear. A tendon can also tear as part of an injury, such as moving or twisting your elbow or shoulder in an awkward way, or falling down with your arm outstretched. At the elbow, the bicep tendon most often tears during the act of lifting a heavy object.
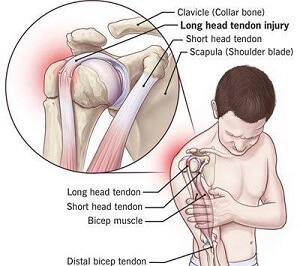
A biceps tendon tear can happen at either the shoulder or the elbow. A tear can also be complete or partial. A complete tear means the tendon has torn away from the bone.
What are the symptoms of a biceps tendon tear?
- Sharp pain at the shoulder or elbow.
- A bruise that appears on the upper arm or forearm near the elbow.
- A feeling of weakness in the shoulder or elbow.
- Trouble rotating your arm from a "palm down" to a "palm up" position.
- A change in the contour of the front of your bicep in the upper arm(“Popeye muscle”).

How are shoulder biceps tears treated?
Surgery may be a choice for those who continue to experience symptoms after non-surgical treatments and have a cosmetic “Popeye” bicep muscle. Surgery to reattach a long head tendon is quite safe, with few complications. It can return nearly all of your arm strength and function, and a re-tearing of the repaired tendon is uncommon.
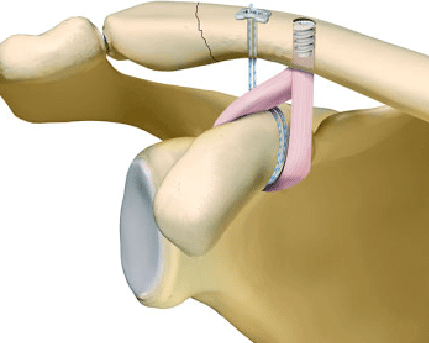
What are distal biceps tendon tears?
While two tendons attach the biceps muscle to the bone at the shoulder, only one tendon attaches it to the elbow. This is called the distal biceps tendon. Tears of the distal biceps tendon are unusual and most often result from an injury or lifting a heavy object. When this tendon tears, however, the tear is usually complete and the muscle is separated from the bone and retracted back. This causes weakness in powerful palm-up activities like tightening with a screwdriver with the right hand.

How is a torn distal biceps tendon treated?
While most people with a torn distal tendon will still be able to move their arms reasonably well, they will usually see a decrease in arm palm-up rotation strength. Because of this, many of them may choose surgical treatment.

It may take three months or more of physical therapy for a surgically repaired distal tendon to heal completely. When it does, patients usually enjoy a full range of motion and near-normal arm strength.
What is Frozen shoulder?
Frozen shoulder or adhesive capsulitis, causes pain and stiffness in the shoulder. Over time, the shoulder becomes very hard to move.
After a period of worsening symptoms, frozen shoulder tends to get better, although full recovery may take up to 3 years.
Frozen shoulder most commonly affects people between the ages of 40 and 60, and occurs in women more often than men. People with diabetes are at an increased risk for developing frozen shoulder.
In frozen shoulder, the shoulder capsule thickens and becomes stiff and tight. Thick bands of tissue — called adhesions — develop. In many cases, there is less synovial fluid in the joint.
Causes
The causes of frozen shoulder are not fully understood. A few factors may put one at more risk of developing a frozen shoulder.
- Diabetes:
- Other diseases:
- Immobilization:
Frozen shoulder occurs much more often in people with diabetes. Diabetic patients with frozen shoulder tend to have a greater degree of stiffness that continues for a longer time.
Some additional medical problems associated with frozen shoulder include hypothyroidism, hyperthyroidism, Parkinson's disease, and cardiac disease.
Frozen shoulder can develop after a shoulder has been immobilized for a period of time due to surgery, a fracture, or other injury.
Treatment
Usually a frozen shoulder is satisfactorily treated conservatively by analgesics (Pain killer drugs), physiotherapy, a local steroid injection, or manipulation under anaesthesia. However, in those cases where conservative management do not produce satisfactory resolution, an Arthroscopic capsular release is the treatment of choice where the tight capsule of shoulder joint is released using pencil sized endoscopic instruments.
Recovery
After surgery, physical therapy is necessary to maintain the motion that was achieved with surgery. Recovery may take 6 weeks to 3 months.
Long-term outcomes after surgery are generally good, with most patients having reduced or no pain and improved range of motion. In some cases, however, even after several years, the motion does not return completely and some degree of stiffness remains. Although uncommon, frozen shoulder can recur, especially if a contributing factor like diabetes is still present.
Subacromial Impingement Syndrome
When the arm is raised to Shoulder height, the space between the acromion and rotator cuff narrows. The acromion may rub against (or "impinge" on) the tendon and the bursa, causing irritation and pain. This is subacromial impingement syndrome.
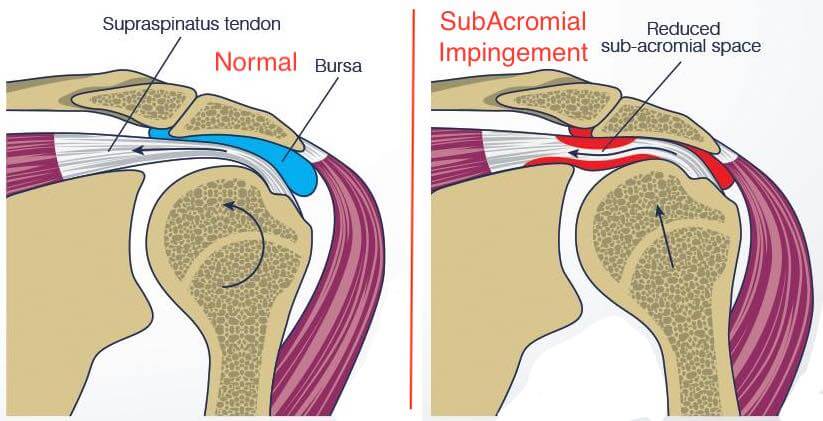
Causes
Those who use their arms overhead for swimming, baseball, and tennis are particularly vulnerable. Those who do repetitive lifting or overhead activities using the arm, such as paper hanging, construction, or painting are also susceptible. Pain may also develop as the result of a minor injury or at times even without apparent cause.
Symptoms
Mild or early symptoms:- Minor pain that is present both with activity and at rest
- Pain radiating from the front of the shoulder to the side of the arm
- Sudden pain with lifting and reaching movements
- Athletes in overhead sports may have pain when throwing or serving a tennis ball
As the problem progresses, the symptoms increase:
- Pain at night
- Loss of strength and motion
- Difficulty doing activities that place the arm behind the back, such as buttoning or zippering
If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.
Treatment
In most cases, initial treatment is nonsurgical like Rest, Analgesics (Painkillers), Physiotherapy, Steroid injection locally etc. However, when non-surgical treatment does not relieve pain, Arthroscopic Subacromial Decompression may be recommended especially if it is associated with rotator cuff tendinitis or tear. In this procedure the surgeon ‘Decompresses” the subacromial space by removing any bony spurs ‘impinging’ on cuff through keyhole surgical incisions and using an arthroscope. Other existing pathologies like cuff tear or biceps tendinopathy etc also are usually addressed along with Subacromial Decompression arthroscopically.
Rehabilitation
After surgery, the arm may be placed in a sling for a short period of time. As soon as comfort allows, the sling is removed to begin exercise and use of the arm. A customised rehabilitation program is provided based on patient’s needs and the findings at surgery. This includes exercises to regain range of motion of the shoulder and strength of the arm. It typically takes 2 to 4 months to achieve complete relief of pain, but at times it may take up to a year.
Loose bodies in Shoulder Joint
Loose bodies are small fragments of detached bone or cartilage that float in the joint thereby causing catching or locking in the joints. Sports or work injuries are the most common causes of loose bodies, however some diseases like Synovial Chondromatosis, Osteoarthritis etc can cause loose bodies in shoulder joint. These diseases are often found in people who use one or more of their joints an extraordinary amount, such as athletes or people whose jobs require extensive lifting, particularly overhead.
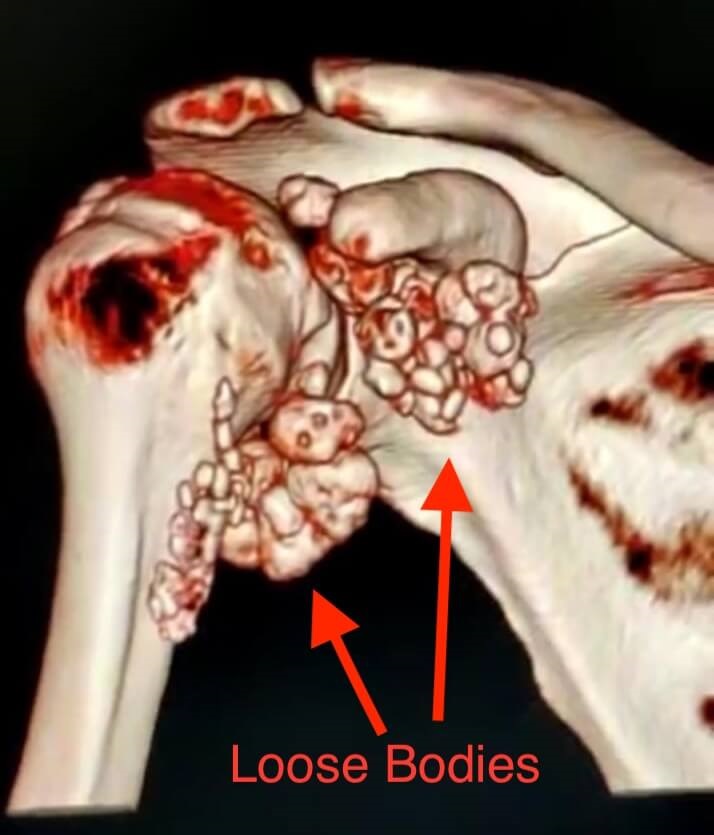
Diagnosis
Clinically a loose body can create a feeling of locking in a person’s joint. The loose particles make it difficult to move the joint. Xray, CT scan, MRI are the investigations often advised by surgeon to diagnose the presence of loose bodies in the joint and their precise location.

Treatment
The aim of treatment is to remove the cartilage or bone that has broken free during injuries and has caused the joints to be less mobile. Most loose body removal procedures are done arthroscopically, which is done with minimally invasive technique using keyhole incisions, has least complications and allows early post-operative recovery.


Fracture of Greater Tuberosity of Humerus
The greater tuberosity is the prominent area of bone at the top of the humerus and is the attachment for the two large, powerful rotator cuff muscles – supraspinatus and infraspinatus.
It is injured/fractured in a fall by either landing directly onto the side of your shoulder or landing with your arm outstretched. It may fracture alone, or with other injuries of the shoulder joint (commonly a shoulder dislocation or complex humeral fracture).
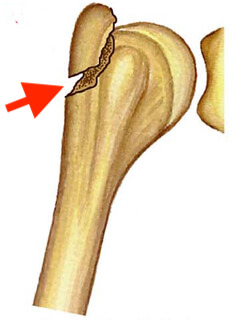
As with most fractures it may be displaced (out of its normal position) or undisplaced.
Treatment
Undisplaced fractures or those fractures which get reduced by closed means after reduction of concomitant shoulder dislocation can be treated conservatively by immobilisation. However those fractures which are displaced require surgical fixation either open method or arthroscopically, so that the function of attached rotator cuff remains intact.
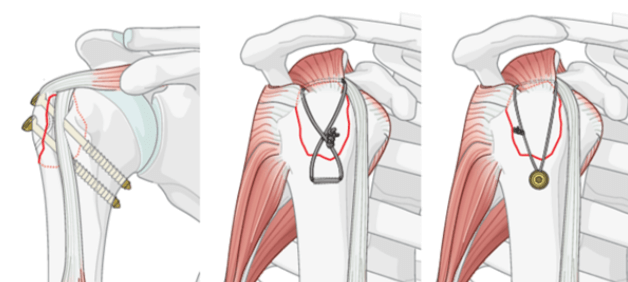
Acromioclavicular Joint Separation
An acromioclavicular (AC) joint separation, is a very frequent injury among physically active people. In this injury the clavicle (collar bone) separates from the scapula(shoulder blade). It is commonly caused by a fall directly on the "point" of the shoulder or a direct blow received in a contact sport. AC joint separations are most common in contact sports, such as football and hockey.
In general, most AC injuries don't require surgery. There are certain situations, however, in which surgery may be necessary. Most patients recover with full function of the shoulder. The period of disability and discomfort ranges from a few days to 12 weeks depending on the severity of the separation. Disruption of the AC joint results in pain and instability in the entire shoulder and arm.


Grades and treatment of AC Separation
There are a total of six grades of severity of AC separations. Grades I-III are the most common. Grades IV-VI are very uncommon and are usually the result of a very high-energy injury such as one that might occur in a motor vehicle accident. Grades I-III can be treated non-operatively whereas Grades IV-VI are all treated surgically because of the severe disruption of all the ligamentous support for the arm and shoulder.
A variety of surgical methods have been used to stabilize a separated AC joint namely:- a fixation across the acromioclavicular space with pins or plates.
- loop fixation from the clavicle to the coracoid process using synthetic materials in acute case or a tendon graft in chronic case.
- Use of a screw or suture loop to stabilize the joint.
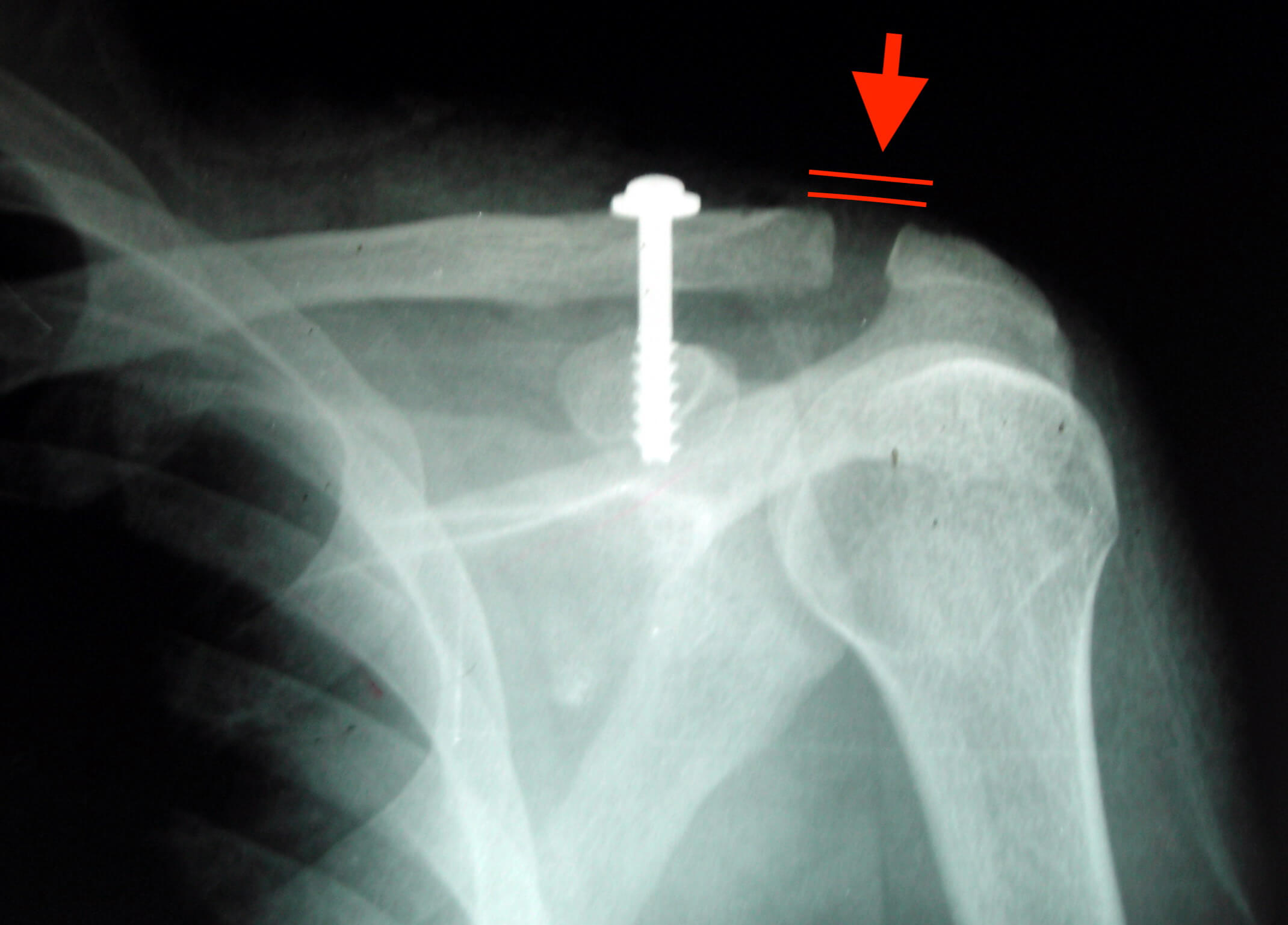
Recovery
Specific recovery programs following surgical reconstruction of the AC joint vary depending on the type of surgery performed. General care recommendations include:
- The use of a sling is required for about 4 weeks.
- Lower arm exercises may begin immediately. With an open surgical technique the arm may be immobilized for 2-3 weeks before motion exercises are begun.
- No weight lifting for 3 weeks.
- Overhead motion is limited for the first 8-12 weeks.
- The patient is allowed use of the arm at waist height to write or perform computer work for the first 12 weeks after which aggressive range of motion and strengthening exercises are started.
- After the removal of the sling, 6-8 weeks of physical therapy is necessary to regain full motion.
- Strength and velocity motions may be delayed for 4-6 months.
Suprascapular Nerve Decompression
Suprascapular nerve is a mixed (sensory and motor) nerve that arises from the upper trunk of the brachial plexus. The nerve travels through the suprascapular notch beneath the superior transverse scapular ligament (STSL) of the shoulder and supplies the supraspinatus and infraspinatus muscles. The primary function of these muscles is to help arm movements at the shoulder joint.
Any injury or compression of the suprascapular nerve results in suprascapular neuropathy.

Suprascapular Neuropathy is a condition of shoulder pain associated with weakness. It is a common problem in overhead athletes who perform repetitive overhead motions or throwing such as swimming, volley ball, tennis, and weightlifting.
Arthroscopic Suprascapular Nerve Decompression is a minimally invasive surgical technique performed to release the compressed suprascapular nerve.
Indications
- Chronic shoulder pain and weakness
- Atrophy of the shoulder muscles
- Failed conservative treatment measures
Surgical Procedure
Suprascapular Nerve Decompression can be performed surgically with an arthroscopic technique under general anaesthesia.
The surgeon makes small incisions on the top of the shoulder. In one incision, the arthroscope is introduced to view the suprascapular nerve, artery and STSL. Other portal is used for the insertion of surgical instruments. The surgeon dissects the nerve and artery from the STSL (Superior Transverse Scapular Ligament). The ligament is sectioned and the nerve is decompressed.The benefits of arthroscopy are smaller incisions, faster healing, a more rapid recovery, shorter rehabilitation period, and less scarring.
Recovery
Post operatively shoulder sling is applied for 2-3 weeks. A rehabilitation protocol is explained to the patient depending upon his needs. Return to normal activities is allowed once the patient feels comfortable with pain.
Shoulder (Paralabral) cysts
Paralabral cysts are swellings that arise around the socket of the shoulder joint (glenoid). They are pockets of joint fluid that develop outside of the joint under tears of the labrum. These are also known as ganglia (or a ganglion). These may occur anywhere around the glenoid.
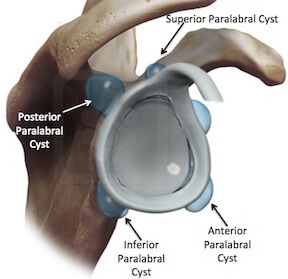
The cysts can be diagnosed on an MRI scan, or MR Arthrogram
Often the cysts themselves don't cause any pain, but the labral tears can cause pain. The cysts may become very large and can press on some of the important nerves around the shoulder. This can cause pain and also weakness of the muscles supplied by the nerve. Treatment involves repair of the labral tear and drainage of the cyst. This is usually done by arthroscopy.
Disclaimer
The information provided on this website is to give a general understanding of the arthroscopic procedures to the patients. It is not intended to substitute any of the published literature in the standard medical textbooks or journals. For more understanding of your medical condition please discuss with the doctor in person at the time of consultation.