Knee Arthroscopy Surgery
With technological advances, Knee Arthroscopy Surgery has evolved and progressed to such an extent that we are able to treat number of clinical conditions more effectively than ever before. It provides better surgical precision, better cosmesis, rapid recovery and thereby more patient satisfaction.
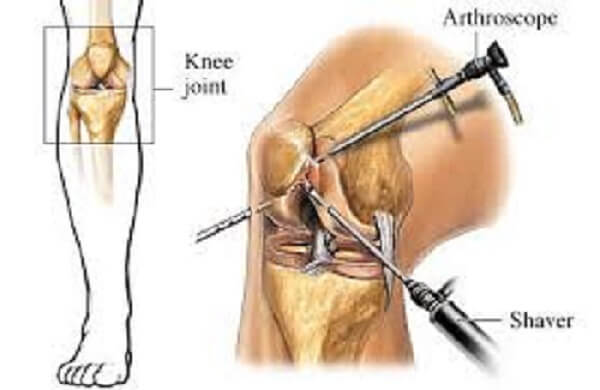
Following are the indications for Knee Arthroscopy Surgery:
- ACL reconstruction surgery
- PCL Reconstruction Surgery
- MPFL Reconstruction Surgery
- MCL Reconstruction Surgery
- PLC Reconstruction Surgery
- Multiligament knee injury
- Medial and lateral meniscus repair or excision
- Osteochondritis dissecans (Cartilage damage)
- Synovitis (Inflammation of cartilage tissue)
- Patellar clunk syndrome (Post total knee replacement)
Arthroscopic knee surgery cost
Arthroscopy Knee Surgery costs depends on the treatment your doctor recommend to you.
The starting price for the same is Rs. 30,000, and it can go up to Rs. 200,000. You must be thinking why the cost is so high; it is all because of the latest technology and equipments used in the process, which is not available at all hospitals easily with highly qualified Arthroscopic surgeon.
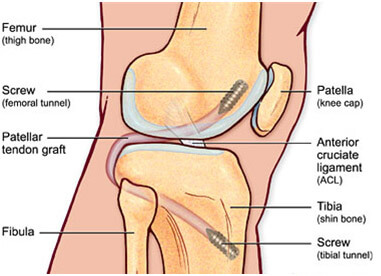
What is ACL reconstruction surgery?
ACL reconstruction surgery is surgery to replace a torn anterior cruciate ligament (ACL) — a major ligament in the knee. ACL injuries most commonly occur during sports that involve sudden stops and changes in direction — such as in football, Kabaddi, downhill running or cycling and gymnastics etc. In ACL reconstruction surgery, the torn ligament is removed and replaced with a piece of similar tissue from another part of your knee. This surgery is performed through buttonhole incisions around the knee joint.
Why is ACL reconstruction surgery done?
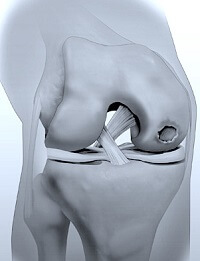
ACL is one of two ligaments that crosses the middle of the knee and connects the thighbone (femur) to shinbone (tibia) and helps stabilize the knee joint.
Most ACL injuries happen during sports and fitness activities that can put stress on the knee:
- Suddenly slowing down and changing direction
- Pivoting with foot firmly planted
- Landing from a jump incorrectly
- Stopping suddenly
- Receiving a direct blow to the knee

ACL reconstruction surgery is generally recommended if:
- The patient is an athlete and wants to continue the sport, especially if the sport involves jumping, cutting or pivoting
- More than one ligament or the meniscus in the knee is injured
- The injury is causing the knee to buckle during everyday activities
- The patient is young
During the procedure of ACL reconstruction surgery
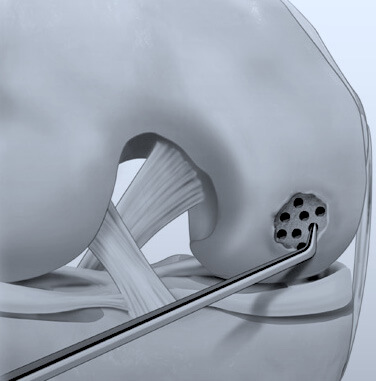
The surgeon will remove your damaged ligament, and then replace it with a segment of graft that comes from another part of the knee. The surgeon will drill sockets or tunnels into the thighbone and shinbone to accurately position the graft, which is then secured to the bones with screws or other fixation devices. The graft serves as scaffolding on which new ligament tissue can grow.
After the procedure of ACL reconstruction surgery
Once the patient recovers from the anaesthesia, he can go home later that same day. The surgeon may ask patient to wear a knee brace or splint to help protect the graft. The doctor gives specific instructions on how to control swelling and pain after surgery. In general, it's important to keep the leg elevated, apply ice to the knee and rest as much as possible. Appropriate medications are prescribed to the patient in the post-operative period. The patient needs to follow his surgeon's advice on when to ice the knee, how long to use crutches and when it's safe to bear weight on the knee. He is also instructed when he can shower or bathe, when he should change dressings on the wound, and how to manage post-surgery care. Progressive physical therapy after ACL surgery helps to strengthen the muscles around the knee and improve flexibility. A physical therapist will teach how to do exercises that the patient will perform either with continued supervision or at home. Following the rehabilitation plan is important for proper healing and achieving the best possible outcomes.
ACL reconstruction surgery results
Successful ACL reconstruction surgery paired with focused rehabilitation can usually restore stability and function to the knee. Within the first few weeks after surgery, one should strive to regain a range of motion equal to that of the opposite knee. Recovery generally takes about nine months. It may take eight to 12 months or more before athletes can return to their sports.
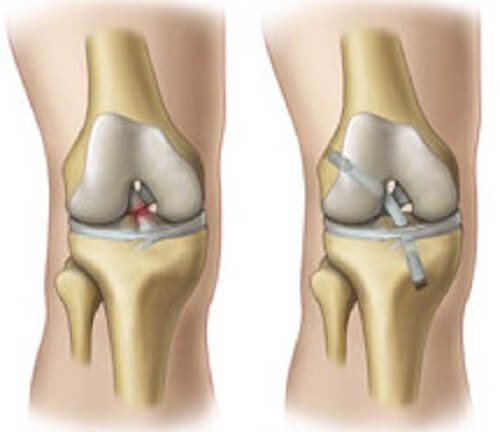
What is PCL reconstruction Surgery?
The PCL is a strong ligament inside the knee. It provides stability against backwardly directed forces on the shin bone. A PCL tear is usually a result of a high velocity injury.
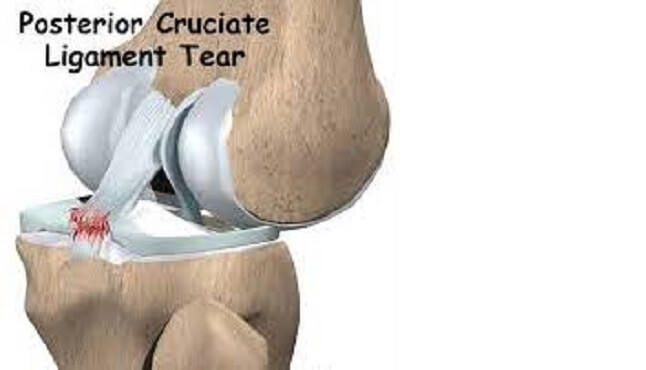
A PCL reconstruction surgery is performed arthroscopically using specialized and highly accurate instrumentation to enable exact recreation of its anatomy. All reconstructive procedures for the PCL require a graft. A common technique involves grafting the torn PCL with segments of the hamstring tendons. If the surgery involves the reconstruction of multiple ligaments at once, different graft materials may be used. In general, most techniques utilise specially designed screws allowing secure immediate fixation of the graft material within bone tunnels drilled into the knee.
How does PCL reconstruction surgery work?
The rationale for treatment is to stabilise an unstable joint, or a potentially unstable joint. Joint stabilisation has been shown to decrease meniscal and articular cartilage injury. This should, in turn, decrease the incidence of later osteoarthritic change. It will also allow return to activities that were difficult secondary to joint instability.
What anaesthesia is used and what are the incisions made?
PCL Reconstruction Surgery is usually performed under spinal, epidural or general anaesthesia. Four incisions approximately 5mm-20mm in length, are made around the knee to place the camera and surgical instruments into the joint, harvest the graft and pass it into the knee. PCL Reconstruction Surgery usually takes between 90 minutes and 2 hours, depending on the complexity of the operation.
How Long does it take to recover?
Crutches are used for comfort, and are usually required for 2 to 4 weeks. Most people are walking reasonably comfortably by 4-6 weeks. It is important not to over-exert too early after the procedure as this can increase discomfort and swelling. Other activities can be gradually reintroduced within ones level of comfort.. People with desk jobs can return to work as early as 1 week, while people in more heavy manual employment may require 6 weeks. The rehabilitation program runs over a 6-12 months or more prior to returning to competitive sports or unrestricted activity.
Is physiotherapy needed after PCL Reconstruction Surgery?
Yes. Although PCL reconstruction surgery has a good probability of returning the knee joint to near normal stability and function, the end result for the patient depends largely upon a satisfactory rehabilitation and the presence of other damage within the joint. Rehabilitation following PCL Reconstruction Surgery is an essential part of full recovery. Ideally this rehabilitation should be carried out under the guidance of a physiotherapist or as explained by the surgeon. Post-operative information will include a rehabilitation program. All rehabilitation programs are flexible. Individual progress varies greatly, and this will require some modifications of the program at the discretion of the surgeon. Different physiotherapy protocols may be used depending on individual needs to meet the described aims.
What is MPFL Reconstruction Surgery?
Medial patella-femoral ligament (MPFL) reconstruction is a procedure used to correct serious and recurring dislocation of the kneecap.
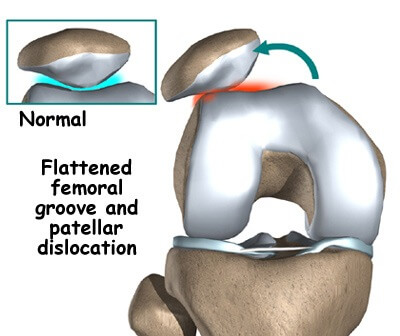
MPFL is the major ligament which stabilizes the patella and helps in preventing patellar subluxation (partial dislocation) or dislocation.
Dislocation can be caused by a direct blow to the knee, twisting injury to the lower leg, strong muscle contraction, or because of a congenital abnormality such as shallow or malformed joint surfaces.
The surgery includes using a ligament taken from elsewhere in the body or a synthetic replacement. The surgeon reconstructs the MPFL to keep the kneecap in the trochlear groove, preventing dislocation.

After surgery, patients will complete physical therapy for 3 to 6 months to ensure the muscles are strong and stable. Patients can expect to return to unrestricted activities by 6 months to 1 year after surgery.
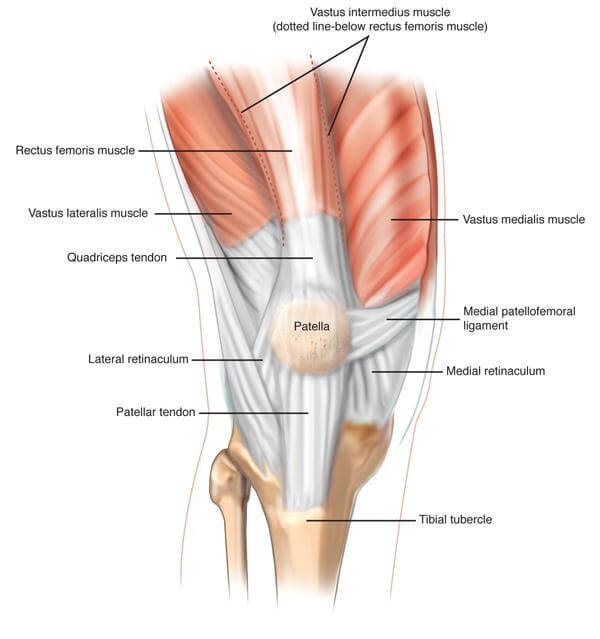
What is MCL Reconstruction Surgery / repair?
The Medial Collateral Ligament (MCL or Tibial Collateral Ligament) is one of the four major ligaments of the Knee. It is on the medial (inner) side of the Knee. It has two parts – superficial and deep.
Medial Collateral Ligament (MCL) Injuries are usually caused by contact on the outside of the Knee thereby pulling apart of this inner structure causing it to tear. Due to very good blood supply an isolated MCL injury tends to heal by conservative (non-surgical) means, however if the MCL is injured along with other ligaments or if the MCL has been avulsed and the tip has slipped inside the joint then it needs surgical treatment. If it’s a fresh injury the MCL is repaired and if it’s an old injury then it is reconstructed using a tendon graft from other part of the leg.
The surgery for MCL is an open surgery. If the operation is done in the acute setting (< 3 weeks after injury), primary repair of the torn ligament is possible.
In cases of chronic (long standing) MCL laxity and instability, MCL Reconstruction Surgery is often necessary. Here a new MCL is prepared from an tendon graft. The new ligament is then fixed at the anatomical MCL site and secured to femur and tibia with fixation devices.
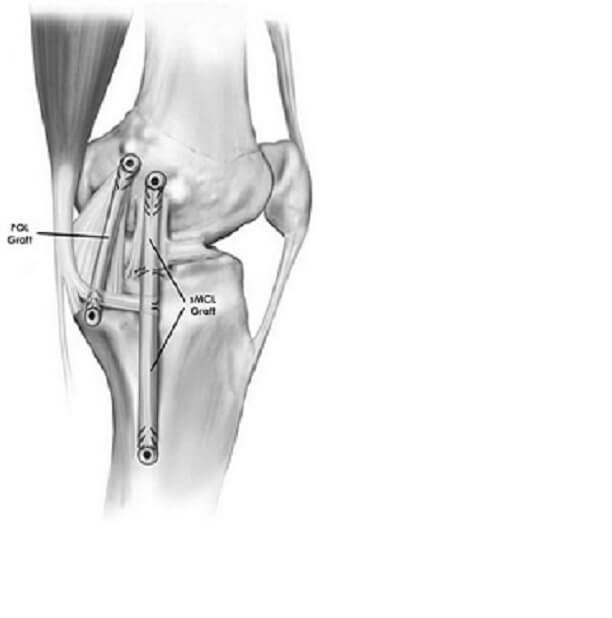
What is PLC repair / reconstruction?
The Posterior-Lateral Corner (PLC) is a part of the knee joint that is located outside and behind the knee, comprising of many ligaments, tendons, and soft tissues. These structures overlap to attach to various structures, and provide static and dynamic stability of the posterior lateral knee.

PLC is torn when posterolateral force is directed to the inside of the Knee, Knee hyperextension, or excessive knee rotation when the Knee is on the ground and partially bent are the causes of injury to the PLC. They frequently occur with other ligament injuries like ACL or PCL.
An isolated grade I or II PLC injury is usually treated conservatively by immobilization of the knee joint in a knee brace followed by physiotherapy after 2-4 weeks. In case of a grade III PLC injury along with other ligament tear within 2 weeks of tear , a repair procedure is done by suturing it end to end or fixing it to the bone using suture anchor.
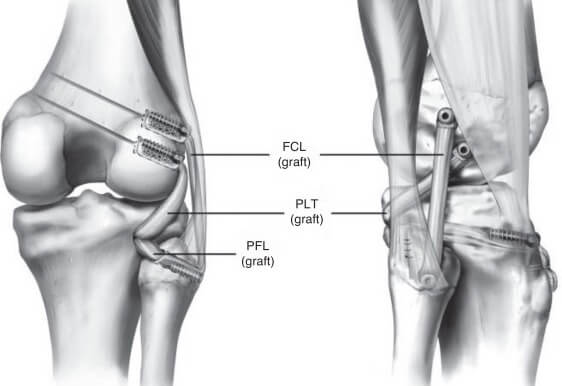
In case of a delayed presentation of PLC injury along with ACL or PCL tear, a reconstructive procedure is preferred in which the PLC is reconstructed using tendon grafts, This is an open complex procedure.
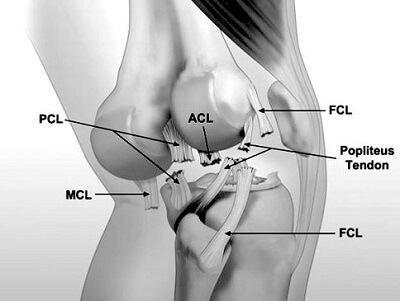
What is multiligament knee injury?
Injury resulting in more than one ligaments of the knee is referred to as a multiligament knee injury. When an injury affecting a combination of the four major knee ligaments—anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL) and lateral collateral ligament (LCL)—occur, the stability of the knee is compromised. Sports-related injuries and trauma are typically the main culprits that cause multiligament knee injuries.
What are the causes and symptoms
Kabaddi, Football, road accidents, fall from height, blow to the knee, and trail running are some common causes of multiligament knee injuries. When the injury results in a tear of several ligaments of the knee, not only does it affect the stability of the knee, but it can also be painful and impede activity.
Symptoms of multiligament knee injuries include:
- Pain
- Swelling
- Disruption in range of motion
- Injury to nerves and arteries of the leg
- Knee instability
Treatment of multiligament knee injury
Usually in case of a multiligament knee injury a personalized treatment plan based on grades of ligaments tear and their combinations is considered by the surgeon. Grades I & II multiligament knee injuries are usually addressed conservatively by a treatment protocol of rest, ice, compression and elevation.
Grade III multiligament injuries require surgery. Moreover, unlike grade III single ligament injury, the surgery is usually performed soon after the injury and often involves more than one surgery.
The surgical reconstruction of damaged knee ligaments is usually performed arthroscopically, however some extra-articular ligaments may need open approach. Arthroscopic surgery involves reconstruction of the torn ligaments utilizing tissue grafts taken from another part of the body.
The damaged ligament is replaced by the graft and fixed to the femur and tibia using metallic or bio-absorbable screws. Gradually, over a period of few months, the graft heals.
After the multiligament knee reconstruction surgery, crutches may be required for up to six to eight weeks, however the recovery depends upon the individual pattern and combination of ligaments injured and also the techniques utilized by the surgeon.
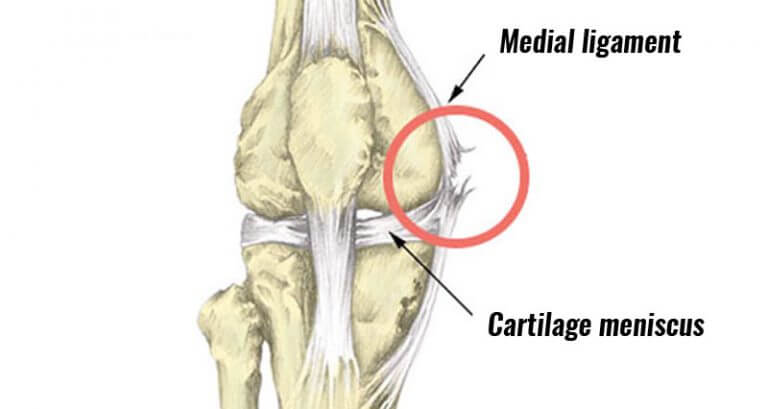
Medial / lateral Meniscus repair/ excision
The meniscus is the soft rubbery cartilage cushion that sits between the thigh bone (femur) and the leg bone (tibia). There are two menisci in the knee; a medial (inside) and a lateral (outside) meniscus. These menisci help dissipate forces across the knee evenly.
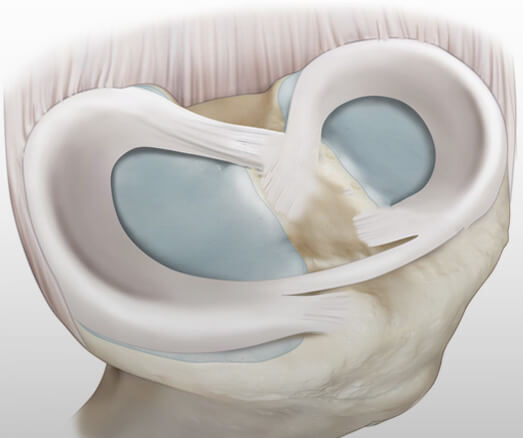
Meniscus injuries are quite common and occur in patients of all ages. An injury can occur as a result of squatting, turning or twisting of the knee. Once the meniscus is torn, symptoms like locking, clicking, swelling and catching are felt by the patient

The pain will be localized along the joint line on the inside or the outside of the knee depending on the tear. The diagnosis is made based upon a history, physical examination and MRI. Most tears are symptomatic and require treatment if they interfere with activities of daily living or sports activities.
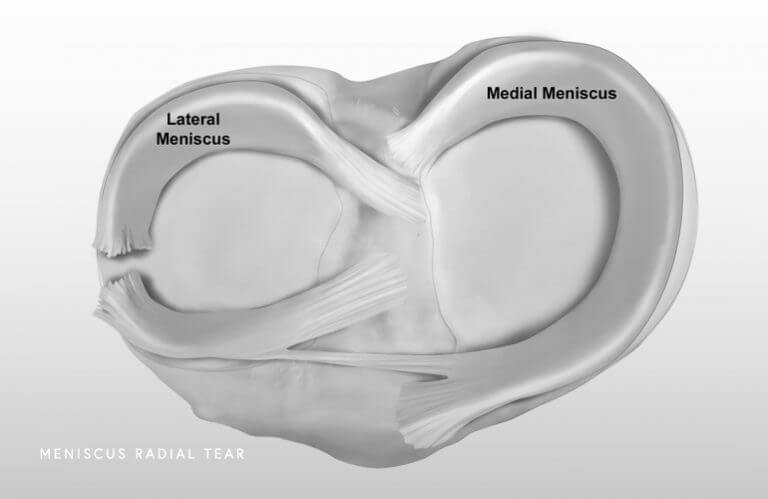
Since the meniscus helps protect the knee from wear and tear, surgeons try to repair the meniscus whenever possible. However, many meniscus tears are not repairable. The meniscus has a limited blood supply, and tears in areas of little or no blood flow have a high risk of not healing. The pattern of the tear is also important. It is not always possible to predict whether a meniscus tear is repairable prior to surgery.
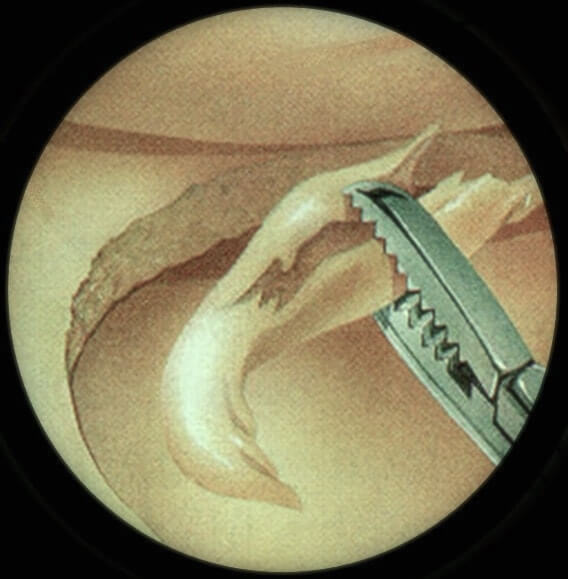
If a meniscus tear is considered appropriate for an attempt at repair, a number of techniques can be used. The procedure is done arthroscopically. A variety of devices or sutures can be used to perform a repair.
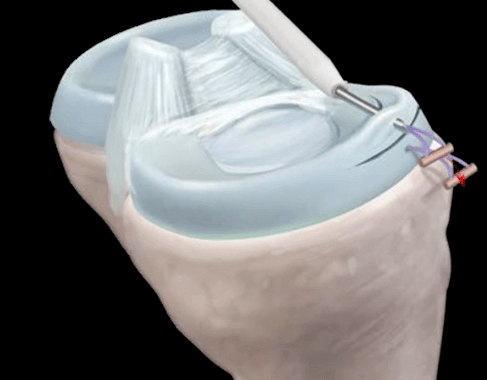

The physical therapy following meniscal repair varies depending on a number of factors. Most patients can put weight on the knee soon after surgery, although a brace may be used. Running is usually delayed until 3-4 months after surgery while a full return to sports and squatting typically occurs after 4-6 months.
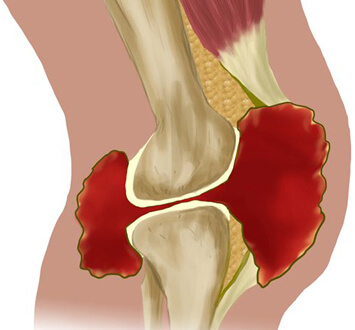
What is Osteochondritis dissecans?
Osteochondritis dissecans is the condition in which bone underneath the cartilage of a joint dies due to lack of blood flow. This bone and cartilage can then break loose, causing pain and possibly hindering joint motion.
Osteochondritis dissecans occurs most often in children and adolescents. It can cause symptoms either after an injury to a joint or after several months of activity, especially high-impact activity such as jumping and running, that affects the joint.
Osteochondritis dissecans is staged according to the size of the injury, whether the fragment is partially or completely detached, and whether the fragment stays in place. If the loosened piece of cartilage and bone stays in place, you may have few or no symptoms. In children it usually heals by itself. Surgery might be necessary if the fragment comes loose and gets caught between the moving joint surfaces or if there is persistent pain
Symptoms
- Pain.
- Swelling and tenderness
- Joint popping or locking - The joint might pop or stick in one position if a loose fragment gets caught between bones during movement
- Decreased range of motion
Causes
The cause of osteochondritis dissecans is unknown. The reduced blood flow to the end of the affected bone might result from repetitive trauma — small, multiple episodes of minor, unrecognized injury that damage the bone. Osteochondritis dissecans occurs most commonly in children and adolescents between the ages of 10 and 20 who are highly active in sports.
Complications
Osteochondritis dissecans increases the risk of developing osteoarthritis of the joint.
Diagnosis
Diagnosis is usually done by physical examination, X-rays, MRI, and/or CT scan
Treatment
Treatment of osteochondritis dissecans is intended to restore the normal functioning of the affected joint and relieve pain, as well as reduce the risk of osteoarthritis. In children whose bones are still growing, the bone defect may heal with a period of rest and protection.
If the patient has a loose fragment in the joint, if the affected area is still present after the bones have stopped growing, or if conservative treatment doesn’t help after four to six months, then the patient might need surgery. The type of surgery will depend on the size and stage of the injury and how mature the bones are. The choice of surgical procedure varies from simple excision of the fragment, microfracturing of the defect, fixation of the fragment if its large enough, transfer of cartilage from non-weight bearing area, to Autologous Chondrocyte Implantation (ACI).

What is Synovitis?
Synovitis (or synovial inflammation) is when the synovium of a joint becomes inflamed (swollen).
The synovium, is connective tissue that lines the inside of the joint capsule. A joint capsule, also called an articular capsule, is a bubble-like structure the surrounds joint. It is composed of a tough, outer layer called the fibrous stratum and a soft inside layer (the synovium). Contained inside both layers is synovial fluid, a viscous liquid that lubricates the joint to reduce friction on the articular cartilage during motion.
Causes of Synovitis
The common causes of synovitis include repetitive stress, rheumatoid arthritis, infections such as tuberculosis, chondromatosis or pigmented villonodular Synovitis (PVNS).
Symptoms
The chief symptom is joint pain. There may not be any visible evidence of injury or swelling that is causing pain. The symptoms are often short-lived and may be felt in different parts of the body at different times. However, when synovitis is caused by overuse of a joint or infection, the pain usually remains in one joint.
Treatment
If the synovitis is unresponsive to conservative management, an arthroscopic synovectomy provides not just the sample for histopathology examination but also a substantial reduction in the disease load.
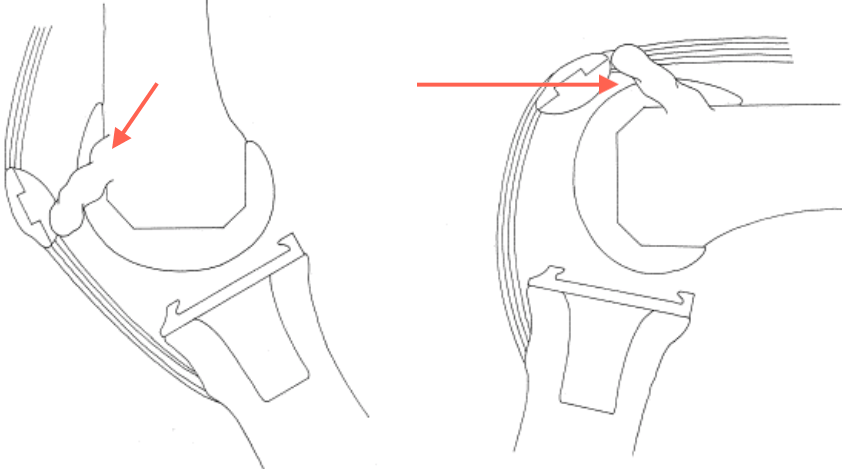
What is Patellar Clunk Syndrome (Post total knee replacement)?
This is a syndrome which occurs when a fibrous nodule forms on the joint capsule, just above the patella. This is a complication of Total Knee Replacement and once this develops the Knee starts making a loud clunk. At about 40 degrees of flexion this lump gets trapped between the anterior flange of the femoral component and hence the clunk. The treatment includes arthroscopic removal of the lump.
Disclaimer
The information provided on this website is to give a general understanding of the arthroscopic procedures to the patients. It is not intended to substitute any of the published literature in the standard medical textbooks or journals. For more understanding of your medical condition please discuss with the doctor in person at the time of consultation.


